Osteoporosis is one of the most widespread degenerative diseases in the world: approximately 20% of men and 50% of women have suffered a broken bone due to osteoporosis yet it remains widely undiagnosed. It is for this reason osteoporosis has been deemed a “silent disease:” most people don’t know they even have it until after they’ve already suffered their first fracture.
Learn How Treatments can Fix a Broken Back
Though they sound terrifying, osteoporotic and neoplastic vertebral compression fractures are actually quite common, and quite painful. How do they happen? When a patient has a degenerative disease like osteoporosis, it causes the bone density to deteriorate. This is especially problematic for the spine because of the weight it carries and its role in the central nervous system. When the structure of a bone fails, it collapses, the other bones above it in the spinal column fall, too—this is known as a compression fracture. Many of these fractures go untreated, leading to a condition known as “kyphosis,” which causes the chest and abdomen to compress and cause serve pain in the back, sides, and ribs. Further, when this condition is treated, it is usually done by way of opioid medication or back braces. Today, we want to present an alternative known as kyphoplasty. What is it and how can it help? Let’s discuss.
Balloon kyphoplasty is a minimally invasive procedure used to treat painful, acute vertebral compression fractures (VCF). During the procedure, the compressed/collapsed vertebrae is filled with a special bone cement to restore the shape and strength of the bone. How? A needle is inserted into the compressed vertebrae. A balloon passes through the needle and inflated. This creates a cavity which gently lifts the bone sections into the normal position. Then the orthopedic cement—technically known as polymethylmethacrylate (or PMMA)— quickly hardens to create an internal cast.
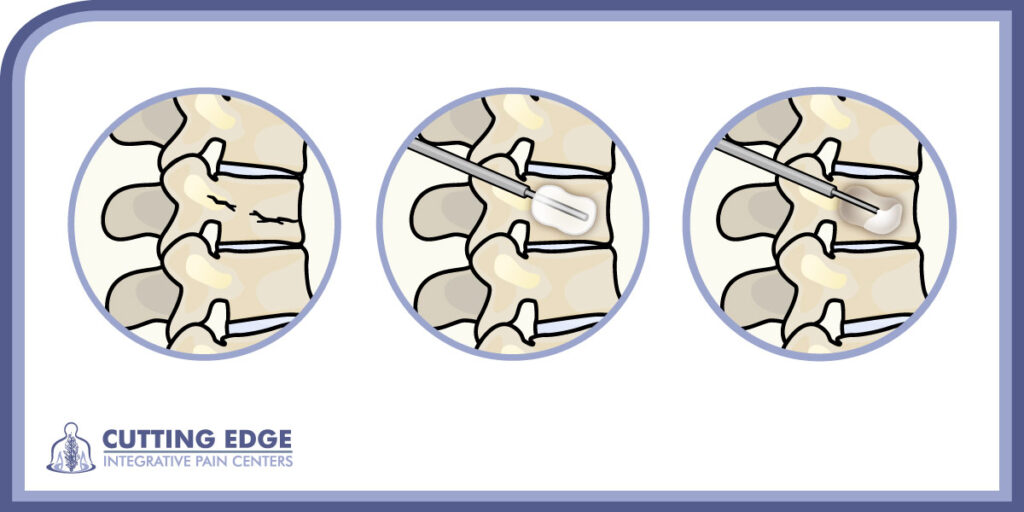
The balloon kyphoplasty procedure lifts the collapsed vertebrae and braces the damaged vertebrae with a special bone cement.
However, there is a continuum of treatments. What we’ve described above (the use of PMMA) is the more traditional method of kyphoplasty. There is, though, a method of using the patient’s own stem cells or concentrated bone marrow for treatment. There are other procedures such as Cortoss, Calcium Phosphate, and stem cell therapy.
There have been upwards of 19,000 scientific articles and numerous studies on kyphoplasty and the results have been overwhelmingly positive. Kyphoplasty is known as a superior osteoporosis treatment for spine treatment and osteoporosis treatment for pain control, while reducing the risk of other fractures, and restoring function. At the time of writing, the procedure already boasts a success rate greater than 70%, though results are improving.
So, what should a pain patient know before deciding whether kyphoplasty is right for them. First, this course of treatment represents an alternative to opioid medication. The patient also does not require any wait time nor bedrest for a back brace because, in essence, the procedure implants a cast directly into the affected vertebrae. This allows for the patient to better return to living a full life, while also avoiding hospital visits.
With reduced pain, disability, medications, and days of limited activities; increased function, quality of life, and ability to take care of oneself, kyphoplasty is a procedure that can help patients suffering from the pain of a compressed vertebrae back to the fulfilling, active life they deserve. There is also no need for a hospital visit, which—given the moment in history we currently find ourselves in—can also provide peace-of-mind for patients.
With all the above-mentioned benefits, it’s clear to see why this procedure is becoming increasingly common. However, if the benefits of the procedure itself weren’t great enough, it may be comforting to a patient to know that kyphoplasty is covered by most insurance providers including Medicare. Further still, recognizing the historical moment we find ourselves living in because of the pandemic, the fact that this is a minimally invasive procedure negates the need for a prolonged hospital stay and reduced exposure to the coronavirus.


